Healthcare Acoustics in New Orleans:
Ochsner Medical Center and the Architects on their behalf requested acoustical consultation services for the West Tower expansion facility as part of the Post Occupancy Evaluation (POE) program. Commercial Acoustics was contracted to perform a sound study within the Neuro ICU on the 7th floor before it is moved to the 9th floor of the West Tower. Commercial Acoustics performed 24-hr site testing and evaluation and is to perform an equivalent study one year after the Unit has been moved and is operational (2019).
The purpose of the testing was to record noise levels for a 24-hr period from within a patient room, as well as to perform spot testing at various locations around the Unit such as nurse stations, corridors, equipment, and other locations. Before the study concluded, six total informal interviews were also conducted with nurses and nursing staff. Commercial Acoustics analyzed these results and raw data as it relates to operations and patient satisfaction (HCAHPS scores).
The findings outlined in the report below discuss the quantitative and qualitative data captured during the performance of these sound studies and discussions.
Commercial Acoustics planned and executed an acoustic study on premises, and completed related research, to outline an appropriate mitigation plan for the hospital noise levels. All measurements in this sound study were completed with a Class 1 Sound Pressure Level (SPL) meter and included time- and spatial-logged data to determine precisely when and where the various noise sources are occurring. Furthermore, all events were classified by type, and any anomalies were noted.
- Documents:
- FGI Guidelines 2010 – Sound and Vibration Design Guidelines for Healthcare Facilities
- An Investigation of Sound Levels on Intensive Care Units with Reference to the WHO Guidelines
- Validating Acoustic Guidelines for Healthcare Facilities
- NIH – Noise in ICUs
- Sleep Deprivation in Critical Illness
- Effects of Intensive Care Unit Noise on Patients: a Study on Coronary Artery Bypass Graft Surgery Patients
- The Role Sleep and Acoustics Play in Creating Safe/Healing Environments of Care
RELATED: See Our Acoustic Consulting Services
Hospital Noise Findings:
There were a number of loud events and critical observations witnessed throughout the 24-hour study. Many of these are listed in Tables 1 and 2 below. These observations were weighted based on their Amplitude (dBA Level) and Repetition (occurrences per hour). A more detailed overview of the criteria and rating system are in Appendix B.
By addressing the key issues with a Weighted Score of 2.5 or higher, Ochsner can expect to see significant improvement in their patients’ sleep quality and sleep-related metrics. The Weighted Score rating system is summarized in Tables 1 and 2 below, and explained in Appendix B.
It should be noted that there are other influential factors in rating the disturbance level of sound. Transient noises that are not rhythmic or consistent can be much more disruptive than louder noises that are repetitive. For instance, a patient may be able to sleep through the constant beep of an IV pump after adjusting to it, but loud chatter in the hallway with an open door may immediately re-awaken the patient1.
Perhaps most importantly is that it is not simply the volume that awakens patients or prevents them from falling asleep. Instead, it is the change in sound level, known as dynamic range. It would be much easier for many people to sleep through a constant 55 dBA sound, than a fluctuating sound between 40 and 55 dBA.
The most disruptive noises in the Ochsner West Tower 7th Floor Sound Study included:
- IV Pumps/Telemetry: Alarms remained at the same level overnight as during the day. Doors of patient rooms remained open, allowing noise from adjacent areas to infiltrate these rooms.
- Nurses and Hospital Staff: Loud talking and joking was observed in the hallways well into the evening (between 9PM and 1 AM), and before 7 AM. There was no observable difference in voice levels between day and night.
- Doors without Closers: Several doors were observed slamming overnight. Lack of door closers allowed doors to slam close even when swinging freely.
The largest underlying issue noticed in the hospital was the lack of a formalized Quiet Hour Policy. Nurses and support staff were unaware of what time the Quiet Hours should begin or end, and any different policies that should be implemented at that time. Lights were turned off at 8:09PM, and back on before 6AM, neither of which correspond with the posted “Visitation Hours” (9AM-9PM). Overhead pages throughout the unit continued past 9PM, and doors remained open. Patient doors typically remained open throughout the 24-hrs, and the number of patient doors open during daytime and nighttime varied very little.
Staff members were observed to be listening to music loudly on multiple speakers in the main nursing area. There were no visual reminders, posters, or cues to enhance Improved Sleeping Efforts, and no Quiet Hour policy against which to enforce behavior.
Hospital Noise Quantitative Findings:
In Tables 1 & 2 below, there were several events throughout the day and evening that contributed to an elevated noise level and varying noises (dynamic range). The tables below summarize the loudness (amplitude) and repetitiveness (# of occurrences) of the observed and measured events. Both factors were considered when prioritizing the overall problematic nature of each source.
A weighting system was used to relate amplitude and repetition for noise occurrences. Each criterion was rated from 1-5, with 5 being the higher weighting (louder, more occurrences). The criteria were combined using the weighting formula outlined in Appendix B to define which sources were most intrusive to patient sleep.
It should be noted that these are not the only important factors. Dynamic Range, representing the changed in sound, and Syntax are important, since people will respond more to their names or certain alarms (telephones) rather than other noises (background Air Conditioning noise).
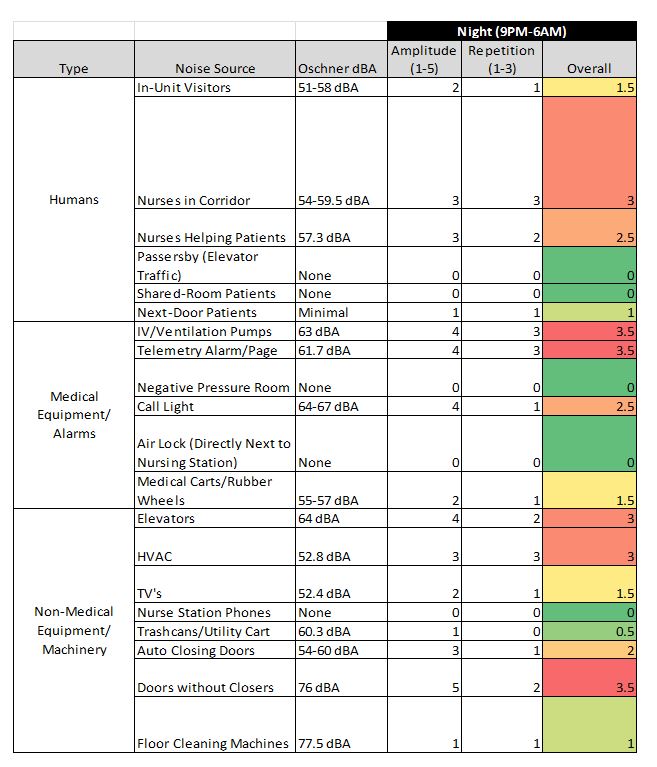
Table 1: Common Noise Contributors during Night Shift
Figure 1 below depicts the noise levels over time for the 24-hr dBA readings in the mock patient room. For the purpose of this study, an office adjacent to the central nurse station was utilized to stage the SPL meter for 24-hr data gathering.
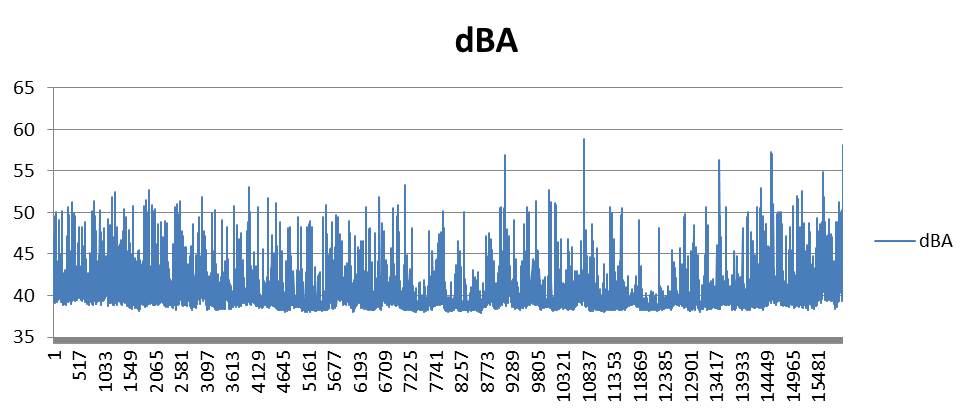
Figure 1: Chart of Sound in Patient Room Closest to Nursing Station
Hospital Sound Solutions:
While there is not a “single” solution to reduce the noise levels experienced by the patients, the most critical elements to address are: Patient Care behavior and communication (affected by training, signage, and reminders), Facility Modifications where necessary, and an integrated Change Management approach.
- Establish Quiet Hour Policies
- Include what should be done at the prescribed time, such as turning off lights and closing doors promptly at 9PM.
- Signage
- There should be at least one sign hung in each entrance (Elevator Bay, Visitor Area, Main Hospital Wing). The sign should have a Call to Action to cue visitors or staff, such as “Please Silence Your Cell Phone”. Furthermore, the more permanent the sign, the higher the level of compliance. The signs should not be taped to the wall, but permanently mounted. (See Appendix C for Example).
- Add Quiet Time Poster at the Main Nurse Station outlining the Quiet Hours Policy.
- Add “Quiet Time” on Green Electronic Signs in hallways.
- Management Involvement
- Hospital Executive Management should perform a midnight check on the wing prior to and after the implementation of the Improved Sleep Program.
- Add Quality Sleep Metrics into the Weekly or Monthly management report so that it is tracked, including HCAHPS noise-related questions.
- Appoint a leader at each level and each unit.
- Other
- Add shades on to windows. Several patients were hanging towels over doors to block unwanted light. A combination of light and sound contribute to lower sleep arousal thresholds.
- Close patient doors, especially at night:
- At 11AM there were 25 open patient doors and 9 closed patient doors.
- At 11pm there were 24 open patient doors and 10 closed patient doors.
- See Appendix A – Raw Notes
- Sensors/Alarms – Investigate options to reduce the dB level on certain alarms. It is clear that this is a safety concern (not hearing a critical alarm when it occurs). However, too many false positive alarms (constant rings and calls from existing stimuli) drown out the critical alarms that may take place. It is extremely unlikely that lowering phone volumes by 5dB will result in missed calls. As other sounds are reduced, these “quieter” alarms will be more audible, but the overall “ambient” volume will be reduced.
- Place “Answer Call” button at doorway of patient room. It is difficult for nurses to get to the Call Button immediately, especially if the patient has started to get out of bed or needs help to the bathroom. Request that nurses hit call button before entering the patient room.
- Facility Improvements
- Outfit all doors with door closers.
- Consider: Implement Sound Masking system into each of the patient rooms to “cover” the sound from the hallway by raising the ambient decibel level within the rooms. When considering the Source-Path-Receiver flow of sound, this would address the Receiver rather than needing to completely eliminate the Source and improve the walls/doors (Path).
- Consider: Light dimming switch for entire unit. 2 of 3 lights should be turned off, and the third light should be dimmed by 50% to provide just enough light to safely maneuver through the hallways.
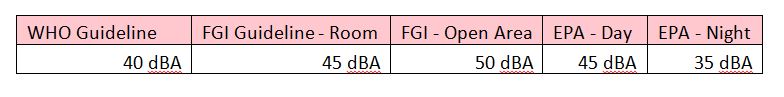
Medical Facility Code Guidelines
For the full report or to schedule a sound study, please contact info@commercial-acoustics.com