Table of Contents
Project Overview: A Behavioral Health Renovation Focused on Emotional Wellness
- Project: Behavioral Health Unit Renovation & Sound Treatment
- Address: 6001 Webb Rd, Tampa, FL 33615
- Facility Type: Behavioral Health Wing – Inpatient Hospital
- Client: HCA West Tampa Hospital
- Contractor: The Robins & Morton Group
- Objective: Support behavioral wellness through intentional design
- Scope: Acoustic ceiling panels across three renovated units
HCA West Tampa Hospital recently invested in the renovation of three behavioral health units to improve patient comfort and clinical effectiveness. The goal wasn’t just renovation—it was transformation. By focusing on sound control, safety, and therapeutic design, the team created spaces that support emotional regulation, recovery, and real healing.
As an acoustic consultant experienced in healthcare environments, we helped identify the right treatments to reduce noise, protect patient privacy, and promote calm. Whether it’s a behavioral health wing or a busy emergency department, our team brings practical, tested solutions that align with both clinical goals and architectural intent.
Inside HCA West Tampa’s Behavioral Health Program
- Behavioral Focus: Offers inpatient psychiatric & mental health care
- Therapy Programs: Includes group sessions, crisis stabilization, aftercare
- Facility Reach: Part of HCA’s statewide behavioral health network
HCA Florida West Tampa Hospital provides critical mental health services to adults in need of short-term stabilization and structured care. Its behavioral health units are designed to balance clinical treatment with a safe, supportive atmosphere—where therapy, daily routines, and quiet environments go hand-in-hand. Renovations to these spaces represent a broader commitment: healing not just through medicine, but through thoughtfully designed environments.

Sensory Considerations & Behavioral Health Design
- Creating Calm: Reduces overstimulation in shared environments
- Group Noise: Echoes in activity rooms increase stress
- Therapy-Ready: Calmer settings improve emotional regulation
Behavioral health units are inherently sensitive to sound. In group settings like dining areas and therapy rooms, echo can quickly escalate stress or trigger emotional reactions. By designing for auditory comfort, hospitals can foster spaces where patients feel safe, grounded, and able to participate in their own recovery.
Creating calm isn’t just about décor—it’s about regulating what people hear and how sound affects them. That’s where architectural acoustics play a direct clinical role.
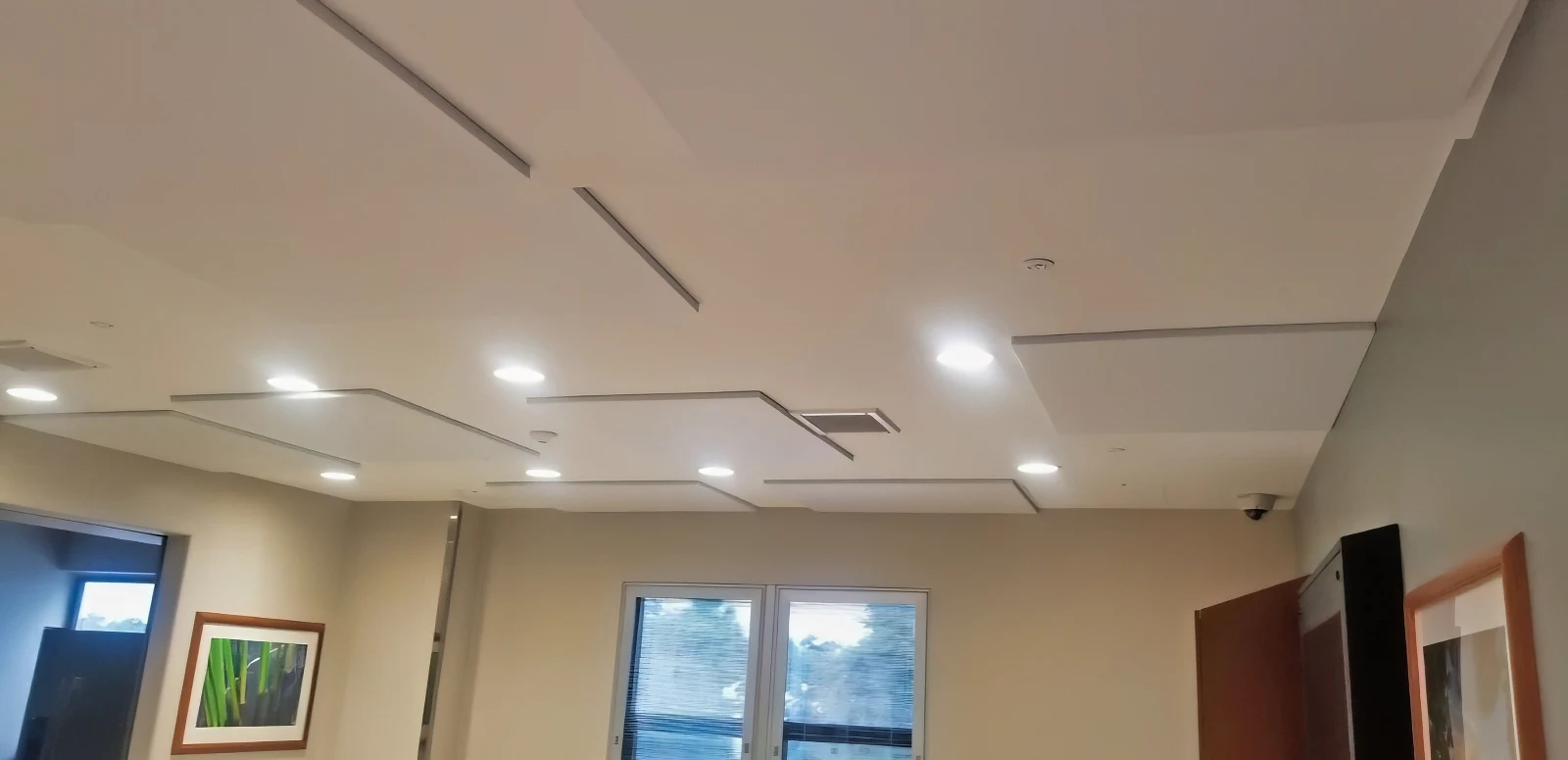
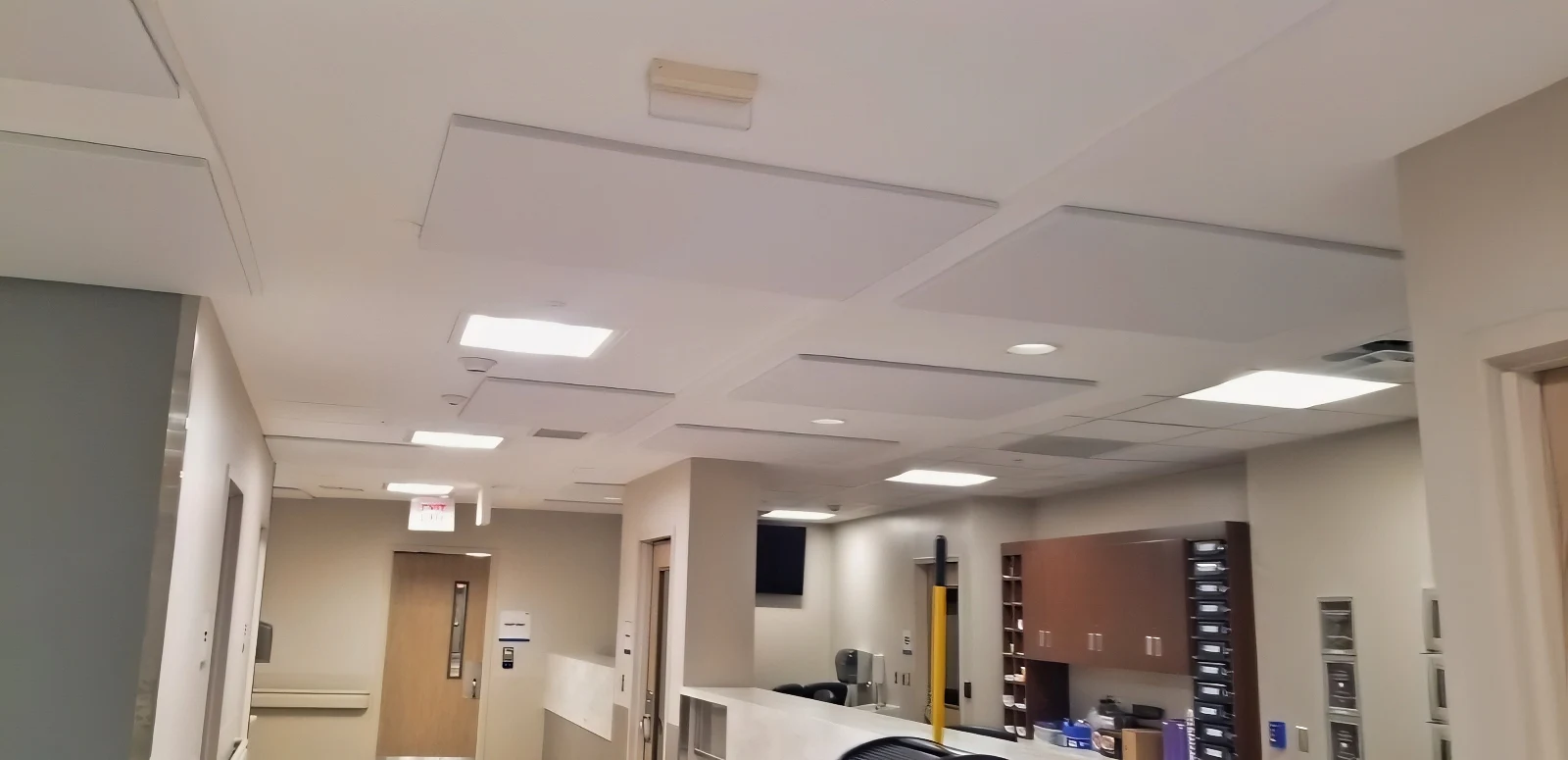
Material Selection & Installation Approach
- PET Panels: Chosen for safety & durability
- Ceiling Mount: Prevents tampering or removal
- Low Profile: White finish blends into ceiling
The design team selected Compressed Polyester (PET) panels instead of standard fabric-wrapped fiberglass. While slightly less absorptive, PET panels are ideal in behavioral health spaces due to their resistance to impact and tampering. These MDC Zintra panels were directly adhered to the ceiling using construction-grade adhesive to ensure a secure and discreet installation.
The white finish helped the panels blend into the existing ceiling surface, maintaining a low-profile look while delivering meaningful echo reduction across each space.

Creating Calm in Group-Based Settings
- Dining Rooms: Large, noisy areas most in need of treatment
- Activity Spaces: Critical zones for group therapy & sessions
- Corridors: High-traffic areas prone to echo buildup
In each of the three behavioral health units, the team targeted areas with the most consistent noise challenges. Dining rooms, activity spaces, and corridors all saw a significant reduction in reverberation once the PET panels were installed.
The result was immediate: patients could engage in group activities with fewer distractions, while staff could guide sessions and routines in a more controlled, peaceful environment. These upgrades directly supported the hospital’s therapeutic goals by creating an environment where calm becomes part of the treatment plan.

Why Sound Matters in Healing Hospital Environments
- Better Sleep: Reduced noise supports rest & recovery
- Staff Efficiency: Quieter spaces improve focus & care delivery
- Therapeutic Value: Sound design supports emotional regulation
Sound isn’t just background—it’s part of the behavioral health strategy. Hospitals that actively manage acoustics are better equipped to deliver whole-person care. Reducing reverberation leads to clearer communication, lower patient agitation, and better staff performance.
When it comes to healing hospital environments, sound control isn’t optional. It’s foundational.

Conclusion: Designing for Emotional Wellness in Healthcare Spaces
The behavioral health renovations at HCA West Tampa Hospital show what’s possible when design and care come together. Working closely with The Robins & Morton Group, the team at Commercial Acoustics delivered a solution that met both safety requirements and therapeutic goals—supporting patients in a calm, structured, and acoustically balanced environment.
For architects and general contractors working on behavioral health projects, this case highlights the value of purposeful acoustic treatment in creating truly healing spaces. If your next healthcare build demands more than just visual polish, it’s time to consider how sound can work in service of wellness.
If you’re planning a behavioral health or hospital project where patient outcomes, staff wellness, and acoustic performance matter, reach out to our team to learn how we can help you create calm, healing environments through expert sound design.

FAQs: Healing Hospital Environments & Behavioral Health Design
How do acoustic treatments support healing hospital environments?
They reduce echo and noise that can trigger stress or agitation—especially in behavioral health settings. By improving speech clarity and minimizing overstimulation, acoustic treatments help create truly healing hospital environments that promote rest, focus, and recovery.
Why were PET panels used instead of fabric-wrapped panels?
PET panels offer a safer, tamper-resistant surface ideal for behavioral health environments while still reducing reverberation. They’re also easy to clean, low-profile, and meet stringent safety requirements for inpatient psychiatric care.
Do ceiling-mounted panels help in behavioral health units?
Yes. Direct-mount ceiling panels eliminate risks from hanging or accessible materials while effectively reducing noise. This makes them an excellent choice for creating calm in sensitive areas like group rooms and corridors.
How does sound affect behavioral health outcomes?
Loud or uncontrolled sound can increase anxiety and interfere with therapy. Sound-treated environments support calm and emotional balance, allowing patients to better engage in care plans and group activities without sensory overload.
Can acoustic design help staff as well as patients?
Absolutely. Quieter environments reduce staff fatigue, improve communication, and create safer, more effective workspaces. In healing hospital environments, good acoustic design supports not only patient well-being but also team performance and job satisfaction.